भारत में शिशु मृत्यु दर में उल्लेखनीय कमी मगर प्रारंभिक नवजात मृत्यु दर और नवजात मृत्यु दर में कोई खास कमी नहीं Revised post
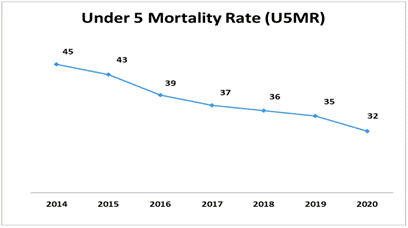
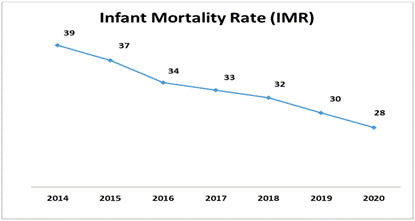
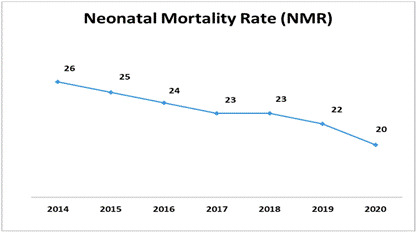
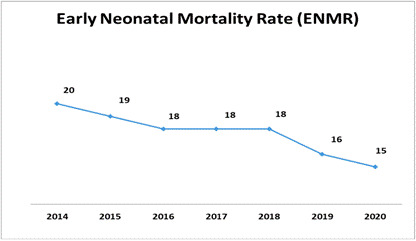
As per the Sample Registration System (SRS) Statistical Report, 2020 released on 22nd September 2022 by the Registrar General of India (RGI), the country has been witnessing a progressive reduction in IMR, U5MR, and NMR since 2014 towards achieving the Sustainable Development Goals (SDG) targets by 2030. ( ALSO READ THE COMMENT AT THE BOTTOM OF THIS POST)
-उत्तराखंड हिमालय ब्यूरो –
नयी दिल्ली, 24 सितम्बर । भारत में शिशु मृत्यु दर में कमी अवश्य आयी है लेकिन अब भी प्रारंभिक नवजात मृत्यु दर और नवजात मृत्यु दर (एनएमआर) में कोई खास कमी नहीं रजिस्ट्रार जनरल ऑफ इंडिया (आरजीआई) द्वारा 22 सितंबर 2022 को जारी नमूना पंजीकरण प्रणाली (एसआरएस) सांख्यिकी रिपोर्ट 2020 के अनुसार देश में 2014 से आईएमआर, यू5एमआर और एनएमआर में कमी आई है और देश 2030 तक सतत विकास लक्ष्य (एसडीजी) प्राप्त करने की दिशा में है।
केंद्रीय स्वास्थ्य और परिवार कल्याण मंत्री डॉ. मनसुख मांडविया ने इस उपलब्धि पर देश को बधाई दी और सभी स्वास्थ्यकर्मियों, सेवा करने वाले लोगों तथा समुदाय के सदस्यों को शिशु मृत्यु दर कम करने में अथक कार्य करने के लिए धन्यवाद दिया। उन्होंने कहा- “एसआरएस 2020 ने 2014 से शिशु मृत्यु दर में लगातार गिरावट दिखाई है। भारत केन्द्रित कार्यक्रमों, मजबूत केंद्र-राज्य साझेदारी तथा सभी स्वास्थ्यकर्मियों के समर्पण से माननीय प्रधानमंत्री नरेन्द्र मोदी जी के नेतृत्व में शिशु मृत्यु दर के 2030 एसडीजी लक्ष्यों को प्राप्त करने के लिए तैयार है।”
| संकेतक | एसआरएस 2014 | एसआरएस 2019 | एसआरएस 2020 |
| अशोधित जन्म दर (सीबीआर) | 21.0 | 19.7 | 19.5 |
| कुल प्रजनन दर | 2.3 | 2.1 | 2.0 |
| प्रारंभिक नवजात मृत्यु दर (ईएनएमआर) – 0- 7 दिन | 20 | 16 | 15 |
| नवजात मृत्यु दर (एनएमआर) | 26 | 22 | 20 |
| शिशु मृत्यु दर (आईएमआर) | 39 | 30 | 28 |
| 5 वर्ष से कम बच्चों की मृत्यु दर (यू5एमआर) | 45 | 35 | 32 |
लगातार गिरावट के बाद आईएमआर, यू5एमआर और एनएमआर में और भी कमी आई है।
देश में पांच वर्ष से कम उम्र के शिशुओं की मृत्यु दर (यू5एमआर) में 2019 से तीन अंकों की (वार्षिक कमी दर 8.6 प्रतिशत) (2019 में प्रति 1,000 जीवित जन्म 35 प्रतिशत की तूलना में 2020 में 32 प्रति 1,000 जीवित जन्म)। इसमें ग्रामीण क्षेत्रों के 36 से शहरी क्षेत्रों में 21 तक का अंतर है।
- बालिकाओं के लिए यू5एमआर बालक (31) की तुलना में अधिक (33) है।
- यू5एमआर में सबसे ज्यादा गिरावट उत्तर प्रदेश (5 अंक) तथा कर्नाटक (5अंक) में देखने को मिली है।
- शिशु मृत्यु दर (आईएमआर) में भी 2019 में प्रति 1000 जीवित जन्मों में 30 से 2020 में प्रति 1000 जीवित जन्मों में 28 के साथ 2 अंकों की गिरावट दर्ज की है (वार्षिक गिरावट दर: 6.7 प्रतिशत)।
o ग्रामीण-शहरी अंतर सीमित होकर 12 अंकों पर आ गया है। (शहरी 19, ग्रामीण -31)
o 2020 में कोई लैंगिक भेद नहीं देखा गया (पुरुष -28, महिला – 28)
- नवजात मृत्यु दर भी दो अंकों की गिरावट आई है। यह 2019 में प्रति 1000 जीवित जन्मों में 22 थी जो 2020 में प्रति 1000 जीवित जन्मों में 20 हो गई। (वार्षिक गिरावट दर: 9.1 प्रतिशत)। यह शहरी क्षेत्रों में 12 से लेकर ग्रामीण क्षेत्रों में 23 तक है।
एसआरएस 2020 रिपोर्ट के अनुसार :
- छह (6) राज्यों/केंद्र शासित प्रदेशों ने पहले ही एनएमआर (<=12 2030 तक) का एसडीजी लक्ष्य प्राप्त कर लिया है: केरल (4), दिल्ली (9), तमिलनाडु (9), महाराष्ट्र (11), जम्मू और कश्मीर (12) और पंजाब (12)
- ग्यारह (11) राज्यों/केंद्र शासित प्रदेशों ने पहले ही यू5एमआर (<=25 तक 2030) का एसडीजी लक्ष्य प्राप्त कर लिया है: केरल (8), तमिलनाडु (13), दिल्ली (14), महाराष्ट्र (18), जम्मू-कश्मीर (17), कर्नाटक ( 21), पंजाब (22), पश्चिम बंगाल (22), तेलंगाना (23), गुजरात (24), और हिमाचल प्रदेश (24)
Most relevant Comment of Ms. Vimla Makhloga on this post: –
————————————————————————————–
The following are the point why IMR is not going low –
1- High-risk pregnant mother identification by ANM/ASHA/AWW is highly neglected
2- ANMs especially in Uttarakhand are attached at headquarters and even ANMs are not visiting the village after posting of ASHA
3- ASHAs are also not informing ANMs of the high risk after several pieces of training
4- Coordination of ANM, ASHA, and AWW is not there
5- Crore of rupees spend in several rounds of training to ASHA on Home Based Neonatal Care and printing material from the state level
6- But ANMs are not being informed in which matter ASHAs has been trained
7- Crores of incentives are being to ASHAs in the name of HBNC but no physical report in HMIS
6- Crore of money spoil in the procurement of HBNC kit of ASHA but approx 10% of ASHA utilized it
8- No monitoring of the Report of HBNC and timely referral is NIL
9- Home Based Neonatal Care i.e. incentive to ASHA, the printing of HBNC form, procurement of HBNC kit forASHA but there is no monitoring system that ASHAs who are getting incentive and certified that they are doing home visits after birth of Children in 3,7,14,21 & 28th day of the childbirth and refer the child to higher institute in case of emergency
10- SNCU and NBSU are nonfunctional staff are not trained in SNCU
11- Pead are posted in low case load hospitals due to political nonwillingness along
12- Rational use of HR as per infrastructure in vain after the launching of NHM in 2005 in the state
13- Under JSSK non availability of free drugs having budget noncoordination of CMO, CMS & Pead, no clear medicine procurement policy
14- Most of the infant deaths are not being reported and in the case of reporting District Collector committee with CMO and Pead review but no action
15- At the state level State Consultant for Mother and Child Care is BDS by profession and in Uttarakhand, most, the of the Consultants in Health are BDS and BAMS, I think they have fewer managerial skills to take reports and review
16- ASHA, ANM, AWW, BPM, DPM, SPM, MOIC, CMO, ACMO, Director NHM, Consultant Mother and Child Care long list but performance Zero due to incoordination, EGO, and political will
17- ASHA, ANM, AWW, and Gram Pradhan is recruited in the name of the Village but they are only taking honorarium in the name of the village actually they are not residing in the village, GOUk has issued GO that those ASHAs who are not residing in the village they will not get annual incentive by the government but everyone is getting
18- ASHA is being supervised by an ASHA facilitator, AF by the Block Coordinator, and Block Coordinator by District Coordinator but all are only facilitating the system by nonperformance
19- AWW are being supervised by Supervisors but 90% of the supervisor even never visit the AWW on the other hand they are taking Rs. 1200 per month TA from the government and ANMs are to be supervised by Health Visitors and Health supervisors but they are only taking Rs. 1200 per month TA, even ASHA facilitators are being paid Rs. 400 visit charges for 20 visits mandatory visits to ASHA but only payment is being done
In this way, crore of the budget is being used only to prevent IMR but it is a great joke and less political will from the government
I was District Program Manager at District Uttarkashi

